General Practitioner doctor Osteoporosis Toolkit
As we look toward 2025, Malaysia faces a looming national crisis: fragility fractures are soaring. With an estimated RM 2.5 billion economic burden, the country faces significant financial challenges. 1 in 3 Malaysian women over 50 are at high risk. The role of the General Practitioner (GP) as the primary gatekeeper has never been more critical.+1
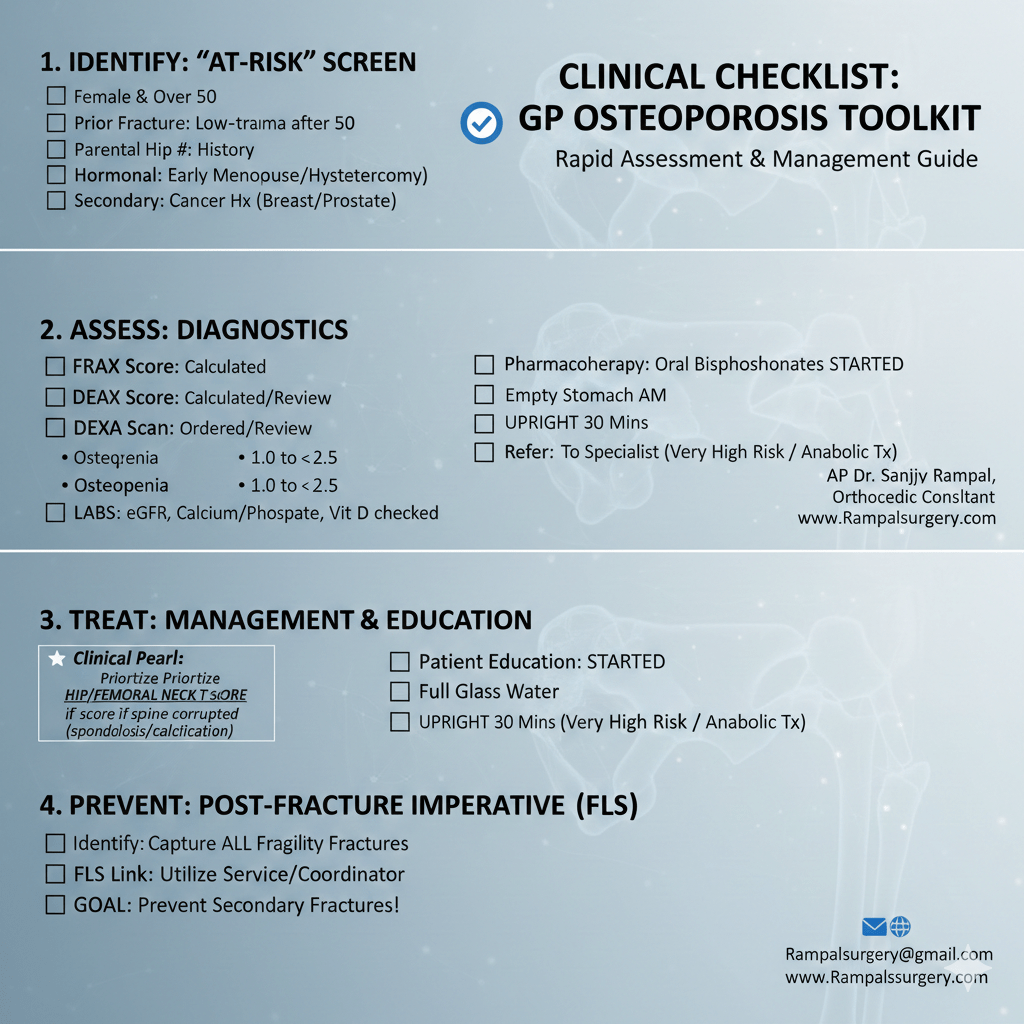
To assist our primary care colleagues, we have developed this High-Impact Clinical Checklist. This toolkit is designed to streamline your workflow, moving from basic calcium supplementation to evidence-based diagnostics and advanced therapeutics.
Why This Toolkit Matters
Osteoporosis is often a “silent epidemic”—detected only after a life-altering fracture occurs. By utilizing a systematic checklist, GPs can:
- Identify high-risk patients early.
- Reduce long-term disability and pain.
- Ensure patients maintain independent living for longer.
The Clinical Checklist: 4 High-Impact Hacks
1. The 1-Minute Screening (Identify)
Don’t wait for a fall. Screen any patient who presents with these “STOP” flags:
- Prior Fracture: Any low-trauma fracture occurring after age 50.
- Parental History: Specifically a history of parental hip fractures.
- Medications: Long-term use of systemic corticosteroids.
- Hormonal Milestones: Early menopause (before age 45) or early hysterectomy/oophorectomy.
- Secondary Risks: History of breast or prostate cancer.
2. Precision Diagnostics (Assess)
Move beyond plain X-rays to specialized assessment tools:
- FRAX Integration: Use the online FRAX calculator (Malaysia-specific) to estimate 10-year fracture probability.
- DEXA Mastery: Interpret T-scores accurately (Normal > -1.0; Osteopenia -1.0 to -2.5; Osteoporosis < -2.5).
- The “Spine Trap”: Be aware that severe spondylosis can falsely elevate spine T-scores. Always prioritize the Hip/Femoral Neck score for an accurate diagnosis.
- Baseline Labs: Always check eGFR, Calcium, Phosphate, and Vitamin D levels before initiating treatment.
3. Stepping Up Treatment (Treat)
Effective management requires more than just a prescription; it requires patient partnership.
- First-Line Oral Bisphosphonates: The cornerstone of primary care treatment.
- Critical Education: Instruct patients to take medication in the morning on an empty stomach. They should use a full glass of water. Patients must remain upright for at least 30 minutes. This ensures compliance and safety.
- Know When to Refer: Patients at “Very High Risk” may require anabolic therapies. These include Teriparatide or Romosozumab. Treatment should be initiated via specialist referral.
4. Secondary Prevention (Prevent)
The “Post-Fracture Imperative” is simple: if they have fractured once, they are highly likely to fracture again.
- Utilize FLS: The Fracture Liaison Service (FLS) model ensures coordinated care. It identifies, investigates, and treats every fracture patient. This aims to prevent the next fracture.
Download the Toolkit
We encourage all GPs to download and print our Clinical Checklist Pocket Card to keep in your consultation rooms. Empowerment through early action is the best way to move “from calcium to care”.
Together, we can strengthen the bones of our nation.

For more information or to discuss a complex case, feel free to contact me at Rampalsurgery@gmail.com or visit www.Rampalsurgery.com.
Leave a comment